Let’s talk about carrots. Sweet and versatile, you can turn them into so many tasty dishes – but the humble carrot has come in for some criticism as of late, with a small yet vocal corner of the internet warning people off them and similarly bright-colored veggies due to fears about “vitamin A toxicity”. We need vitamin A, though, right? Where is this fear coming from, and should we really be viewing carrots with mistrust and suspicion?
What is vitamin A?
Vitamin A is a fat-soluble vitamin that has lots of important functions in the human body. It plays a role in the development and regulation of the immune system; it helps promote good lung function; and perhaps most famously, it’s vital for healthy vision.
Vitamin A deficiency can cause a group of symptoms known as xerophthalmia. Vitamin A helps keep the eyes properly lubricated and is an essential component in the production of pigments in the retina, without which you can develop night blindness, an early sign of vitamin A deficiency. With more severe or long-term deficiency, total vision loss can occur. The World Health Organization estimates that 250,000 to 500,000 children become blind due to vitamin A deficiency every year.
These are just some of this vitamin’s vital roles. Thankfully, there are lots of different dietary sources of vitamin A to help you ensure you’re getting enough.
How do we obtain vitamin A?
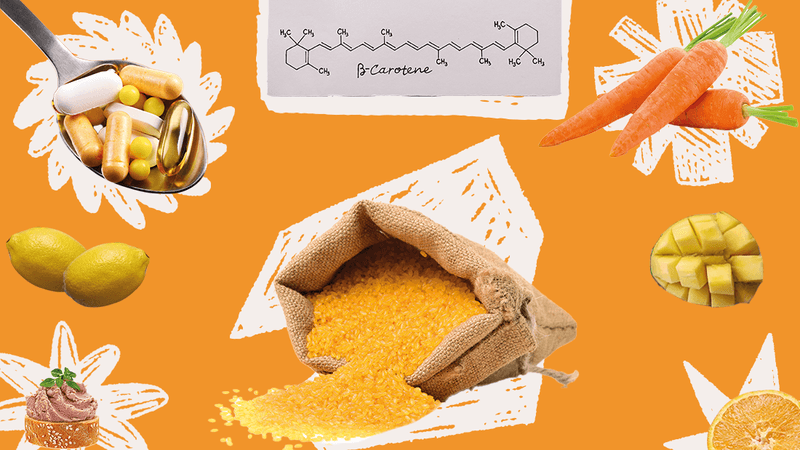
You can get vitamin A from foods in two ways. There’s preformed vitamin A, which is found in fish, offal, dairy products, and eggs. There are also provitamins called carotenoids, which the body can convert to vitamin A as needed. These are found in lots of fruits and vegetables, including carrots – beta-carotene is what gives them their carrot-teristic orange hue (sorry).
Because of the health risks associated with vitamin A deficiency, particularly in areas with high food insecurity, scientists have worked to produce fortified foods with extra carotenoids. The most famous example, Golden Rice, has been shrouded in controversy since its development, with environmental groups stoking unfounded fears around genetically modified organisms (GMOs) and international restrictions on its distribution.
Earlier this year, a court in the Philippines revoked the permit for the commercial production of Golden Rice in the country in a case brought by Greenpeace Southeast Asia and other groups. While the move was heralded as a victory by Greenpeace, there was consternation from many in the scientific community who see blanket opposition to GMOs as holding the world back from solutions to the problem of malnutrition.
In regions where food is less scarce, obtaining enough vitamin A from natural and fortified sources (like breakfast cereals) is possible for most people. For some on very restricted diets, or those with diseases like cystic fibrosis or inflammatory bowel disease that can affect nutrient absorption, a vitamin A supplement may be recommended by a doctor.
This is where things can get a bit dicey. Vitamin A deficiencies are definitely harmful, but so is taking in too much.
What happens if you have too much vitamin A?
Hypervitaminosis A, also called vitamin A toxicity, occurs when you exceed the recommended daily allowance (RDA) of around 700-900 micrograms per day in adults or 300-600 micrograms per day in children.
The toxicity can either be acute or chronic, and arises because the fat-soluble vitamin A accumulates in the liver.
Acute toxicity can occur if you’re exposed to super-high doses in a short amount of time. The symptoms include a severe headache, nausea, dizziness, and blurred vision, as well as rashes and peeling skin.
Chronic hypervitaminosis A, on the other hand, occurs when someone consumes excessive doses – about 10 times the RDA – for several months or sometimes even years. Symptoms include dry skin, cracked lips, muscle and joint pain, fatigue, and hair loss.
In the most severe cases, hypervitaminosis A can be fatal. There are also risks to the fetus if a pregnant person develops hypervitaminosis A.
However, the condition is relatively uncommon. Acute toxicity is normally the result of an accidental overdose. Chronic toxicity is sometimes seen in communities that rely heavily on vitamin A-rich animal livers as a food source. According to BBC Science Focus, only 0.1 grams (0.004 ounces) of polar bear liver would be enough to satisfy an adult’s RDA of vitamin A. The UK’s National Health Service recommends that people only consume liver or pâté once per week.
Another group at higher risk of hypervitaminosis A is those with certain skin conditions, like acne, who are prescribed medications containing retinoids. These are compounds derived from vitamin A; as Dr Brian Wu wrote for DermNet, high-dose vitamin A from skin medications is among the most common causes of chronic vitamin A toxicity. Speak to your dermatologist if you’re concerned about this.
For the average person – presuming you’re not feasting on liver every night – it’s very unlikely that you will be consuming excessive amounts of vitamin A from your diet. Where there could be a risk, however, is from taking supplements without paying close attention to the quantity of vitamin A (and, importantly, the type of vitamin A) they contain. This is particularly problematic for kids, as their smaller bodies can’t tolerate as much as adults can.
It’s always recommended to discuss any supplements you’re planning to take, or give to your kids, with your doctor first – take the bottles along with you so that they can see the labels and check the quantities (but beware: these labels are not always accurate). If you’re really concerned that you or your child might have a vitamin A deficiency, the best option would be to ask for a blood test to check before reaching for supplements.
And what you definitely should not do is modify your entire diet to try and remove any and all colorful things. Strap in: we’re going wrap this up with vitamin A detox diets.
Vitamin A detoxes; or, why regular people should not be afraid of carrots
In a corner of wellness social media, there are people offering tips on how to “detox” from too much vitamin A by eliminating any and all sources of preformed and – this bit’s important – provitamin A from your diet.
The idea of “detox diets” has been debunked time and time again. There’s no diet that can “cleanse” the body, and needlessly restricting your diet is more likely to lead to other vitamin and mineral deficiencies than any positive outcome.
If you are really concerned about the risk of hypervitaminosis A, your first port-of-call should be your doctor, not the grocery store.
But there's another major problem specific to these low vitamin A diet plans: they include provitamin A. These are the carotenoids that are present in many fruits and veggies – back to the carrots again! – which the body can convert to vitamin A. The thing is, the body will only do that if it needs to.
As the National Institutes of Health explains, “High intakes of beta-carotene do not cause the same problems as preformed vitamin A.” In other words, you can eat pretty much all the carrots you like – it’s not going to cause a vitamin A overdose. What it might do is turn your skin orange, thanks to a condition called carotenemia. This is usually harmless and reversible, but still best avoided (and probably a sign that you should diversify your veggie consumption a bit).
Put simply, there’s no reason for the average person to be concerned about eating too many carotenoids. You can safely ignore those people on TikTok and continue with the usual tried-and-true advice to aim for as balanced a diet as possible.
It might not sound as sexy, but at least you won’t have to scour the farmer’s market for white carrots.
The content of this article is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of qualified health providers with questions you may have regarding medical conditions.
All “explainer” articles are confirmed by fact checkers to be correct at time of publishing. Text, images, and links may be edited, removed, or added to at a later date to keep information current.